Lymphadenopathy in children: a diagnostic dilemma
This website presents an oversight of novel research into a more targeted and non-invasive diagnostic approach of children with cervical lymphadenopathy suspected of lymphoma. With the absence of a medical guideline, we aim to make a significant impact for early detection of high-grade lymphomas. In parallel, we aspire to reduce the number of unnecessary referrals and biopsies for children with benign conditions.
Method of data-driven approach
We collected data from all children with cervical lymphadenopathy referred
to our national pediatric oncology center within 30 months (n = 182). We identified 39 potential predictors based on an extensive search of the literature. We used pathology reports for defining the diagnosis.
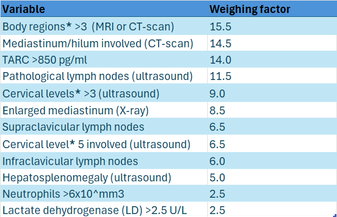
First, we preformed univariate analysis. A p-value of <0.01 was considered statistically significant. Hereafter, we integrated the best univariate predicting factors into a multivariate, machine learning logistic regression model using Python Programming software (version 3.8.8). We only included variables which can be used in general clinical practice.
Machine learning makes it possible to uncover patterns, construct models, and make predictions by learning from training data. It also provides removal of human bias in decisions. This approach utilizes the best combination of variables. Logistic regression allocated each variable a weighing factor. After finishing the multivariate model, the model was tested in a different patient cohort (n = 60).
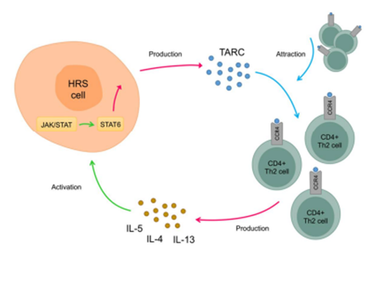
Thymus and Activation-Regulated Chemokine (TARC)
Thymus and activation-regulated chemokine (TARC) is produced by different cell types and is highly expressed in the thymus. It plays an important role in T-cell development, trafficking and activation. Importantly, TARC is also produced by malignant Hodgkin and Reed-Sternberg (HRS) cells of classical Hodgkin lymphoma (cHL). In cHL, HRS cells survive and proliferate due to the micro-environment consisting primarily of type 2 T-helper (Th2) cells. TARC-mediated signaling initiates a positive feedback loop that is crucial for the interaction between HRS and T cells. The clinical applicability of TARC is diverse. TARC is a useful diagnostic biomarker in both children and adults with cHL and in other Th2-driven diseases.
In children with lymphoma, classical Hodgkin lymphoma (cHL) is most prevalent. Therefore it is very convenient to implement this biomarker in our scoringstool.
Scoring tool
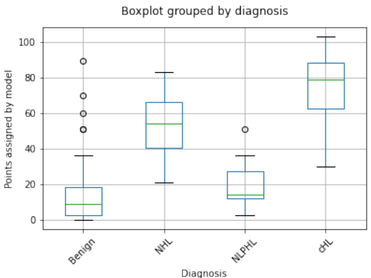
We report a 12-factor diagnostic model with a sensitivity of 95% (95% CI 89–98%) and a specificity of 88% (95% CI 77–94%) for detecting classical Hodgkin Lymphoma (cHL) and Non-Hodgkin Lymphoma (NHL).
The tool is based on data of children referred to a children's oncologist. It is unknown if these numbers apply on the patient population visiting the general pediatrician.
Based on these data, we suggest that children with a score of 27.5 or higher should be referred to a pediatric oncologist.
The diagnostic model could discriminate excellently (p < 0.001) between the benign group (median 9.0, 25–75 percentiles 2.5–18.0 points) and the cHL group (median 78.0, 25–75 percentiles 62.0–87.0 points) and between the benign group and NHL group (median 54.0, 25–75 percentiles 40.0–65.5). The model could not discriminate between nodular lymphocyte-predominant Hodgkin lymphoma (NLPHL) and the benign group.
* Specification of different localizations that were scored separately:
- Nodal involvement: upper cervical, supraclavicular, infraclavicular, retro auricular or pre auricular Waldeyer’s ring, mediastinum/hilar, thoracic wall, porta hepatis, renal hilum, splenic hilum, and other abdominal lymph nodes (para-aortic, para-iliacal and mesenteric) and inguinal lymph nodes.
- Extranodal involvement: thyroid, thymus, lung, liver, spleen, kidney, intestines, testis, bone marrow, bone and other
* Cervical levels scored in accordance with
Robbins Classification
Future plans
This research was a collaboration between Prinses Maxima Centre for children's oncology and Erasmus Medical Centre.
We're in the process of establishing a prospective study to evaluate the applicability of our scoring tool in academic and general pediatric practice. This forthcoming research will determine whether the model should be adjusted or minimized.
Our ultimate aim is to create a national guideline.
Article
Read the article published in Cancers discussing significant advancements in the evaluation of cervical lymphadenopathy in children.